Imagine an outbreak of a disease like SARS (severe acute respiratory syndrome) that will likely become an epidemic affecting thousands of people. Wouldn’t it be helpful to know early in the epidemic how fast the disease would spread and how many people may be infected so that the medical community could be prepared to treat them?
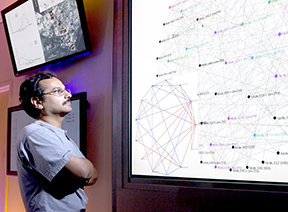
Sandia/California researcher Jaideep Ray (8964) has developed a computer model that can do just that.
In his third year of internal LDRD (Laboratory Directed Research & Development) funding Jaideep has figured out a way to determine the number of people likely to be infected and die from noncommunicable illnesses like anthrax — ailments that could be caused by a potential bioterrorist attack — as well as communicable diseases like smallpox.
“In the past decision makers were only able to observe — watch people get sick, go to the hospital, and maybe die,” Jaideep says. “They had no idea how many people would get sick tomorrow or two days from now.”
He came to this realization in 2004 when he was working on a project for the Department of Defense where he developed a computer model that had decision makers responding to an epidemic at a naval base.
“It struck me that we were going about this completely backwards,” Jaideep says.
He proposed an LDRD where he would develop mathematical tools that, using information from the first days of an epidemic, would estimate how many people were going to get sick during the course of the epidemic.
He spent the next three years working on the software and in the middle of 2007 successfully developed a model that could infer the characteristics of a bioterrorism-related epidemic of a noncommunicable disease like anthrax. These inferences were drawn from observations of people with symptoms of anthrax exposure collected over the first three to five days of the epidemic. He is within a few months of refining a computer model that would do the same for communicable diseases.
Russian anthrax outbreak
Jaideep says that characterizing diseases requires observations of real outbreaks and then building computer models around them. He did this for a 1979 anthrax outbreak in Sverdlovsk, a city of 1.2 million people in western Siberia. Initially the Soviets said the victims got the disease by eating anthrax-contaminated meat or having contact with dead animals. At the end of the Cold War American physicians reviewed documents published by pathologists who performed autopsies during the epidemic, confirming the pathogen was airborne. Records showed that 80 people were infected by inhaling the pathogen. A total of 68 died of the disease.
Using the computer program, Jaideep ran the data obtained from hospital records of people who became sick in the early days of the epidemic. The program automatically tried many combinations of the unknown number of infected people, time, and dose of anthrax exposure until it got as close to the real observation as possible. In the final runs, using data from the first nine days of the 42-day outbreak, the model inferred that almost certainly less than 100 people had been infected, with the most probable number around 55.
That was “pretty close,” to the real event, he says. The program, which also estimated the time of the release and the dose of anthrax inhaled, took 10 minutes to run.
“If they had had this program in 1979, the Soviet officials would have known that this was going to be a small outbreak,” Jaideep says. “Instead they got into a panic and vaccinated 50,000 to 60,000 people — the whole southern end of the city.”
Nigerian smallpox model
After proving the software actually works, he turned his attention to communicable diseases, specifically smallpox. He modeled a documented smallpox outbreak in Nigeria in 1967, which broke out in a fundamentalist sect (Faith Tabernacle Church, FTC) in the town of Abakaliki. The sect consisted of 120 people who lived in nine different compounds, along with 177 of their nonsectarian brethren. The FTC members mixed strongly in their compounds and across compounds at church four times a week and social visits.
A small girl first introduced the disease into the population. It spread rapidly in her compound and jumped to other compounds via the church and social visits. The sect members refused medical treatment and did not quarantine the sick and contagious members. While the World Health Organization (WHO) monitored the outbreak and kept records of who got sick and when, it did not record the dates of recovery or deaths of the infected people.
Of the 32 people who became infected during the epidemic, 30 were FTC members.
“It was clear from the WHO observations that there was strong transmission inside compounds and weaker ones across compounds,” Jaideep says.
Differentiating the communicable disease model from the noncommunicable disease model is the importance of social networks. Communicable diseases spread faster through people in closer proximity. For example, close family members of an infected small child would have a higher probability of contracting the disease than someone who lives in another compound or house.
Jaideep says the challenge is that making inferences about social networks is hard. There is a tendency for the inference mechanism to quickly “settle down” into one of a few possible network configurations. While he estimates that it will take about four to six months to overcome this “stickiness” of the inference mechanism, he has successfully obtained estimates using a few simplifications.
One simplification is to assume a fully connected social network but allow the disease to progress through the population at two different rates, one for in-compound transmission and a smaller one across compounds. Using this approach he inferred the two transmission rates from observations and found the cross-compound transmission to be about four times slower.
A second simplification is to assume there exists only one transmission rate and explain the slower spread across compounds to fewer and unknown “strong” cross-compound social links. Using this second approach, he inferred the transmission rate as well as the cross-compound social links that existed.
Under both simplifications, he also inferred the chains of transmission, that is, the links in the social network along which the disease traveled, infecting people in its wake. Typically, chains of transmission are identified by painstaking contact tracing by epidemiologists.
Once these disease characterization parameters are inferred from data, they can be entered into conventional epidemic models that predict the evolution of the epidemic in the population and predict the number of people getting sick on a given day.
As of today, these inference techniques can work with incomplete observations. Using data from the first 40 days of the three-month epidemic, Jaideep was able to develop “true” characterizations.
”These preliminary results are useful and encouraging,” Jaideep says. “Within a few months we should be able to remove the simplifications and perform inferences with models which are even more reflective of the actual spread of the disease.”