Device detects seizure gases, providing advance warning

In people with epilepsy, seizure-alert dogs can smell small changes in body chemistry and warn of an impending seizure an hour or more before it occurs. Inspired by this feat of nature, a team of researchers has sniffed out a way to replicate the ability with technology.
Sandia and research partner Know Biological Inc. have developed a miniaturized sensor system that can detect the specific gases released from the skin of people with epilepsy before a seizure.
The Sandia-designed device was able to sense the key gases from gauze swiped on a patient’s skin 22 minutes before the onset of a seizure, said Gary Arnold, CEO and founder of Know Biological.
For people who have epilepsy, knowing they will have a seizure in advance gives time to take medication that can halt most seizures or, at the very least, to get somewhere safe and private.
“A friend of mine has epilepsy,” Arnold said. “He told me that having a seizure is horrible but that it’s not the worst part of epilepsy. The worst part of epilepsy is never knowing when you’re going to have a seizure. The psychological impact of that uncertainty is overwhelming.”
How does the nose know?
Arnold and academic collaborators wanted to know how seizure-alert dogs knew when a seizure was imminent. They identified the presence of several key volatile organic compounds, known as VOCs, for the gases responsible for everything from the smell of fresh-cut grass to the odor of drying nail polish. They discovered that seizure-alert dogs know when a seizure is imminent because they smell the change in body chemistry.
“We were able to identify a bouquet of eight VOCs that were unique to seizures,” Arnold added. “Of those, three VOCs were considered principal, appearing in every sample taken from someone having a seizure. These VOCs start building in concentration prior to seizure onset.”
Arnold reached out to Sandia after hearing about work developing a handheld chemical detector for the military. Sandia’s work developing a miniaturized gas detection system began more than 25 years ago as part of a large internal research investment.
Making a silicon “nose”
Arnold and Sandia biomedical engineer Philip Miller have been working on adapting the miniaturized system to detect the gases Arnold’s collaborators had previously identified.
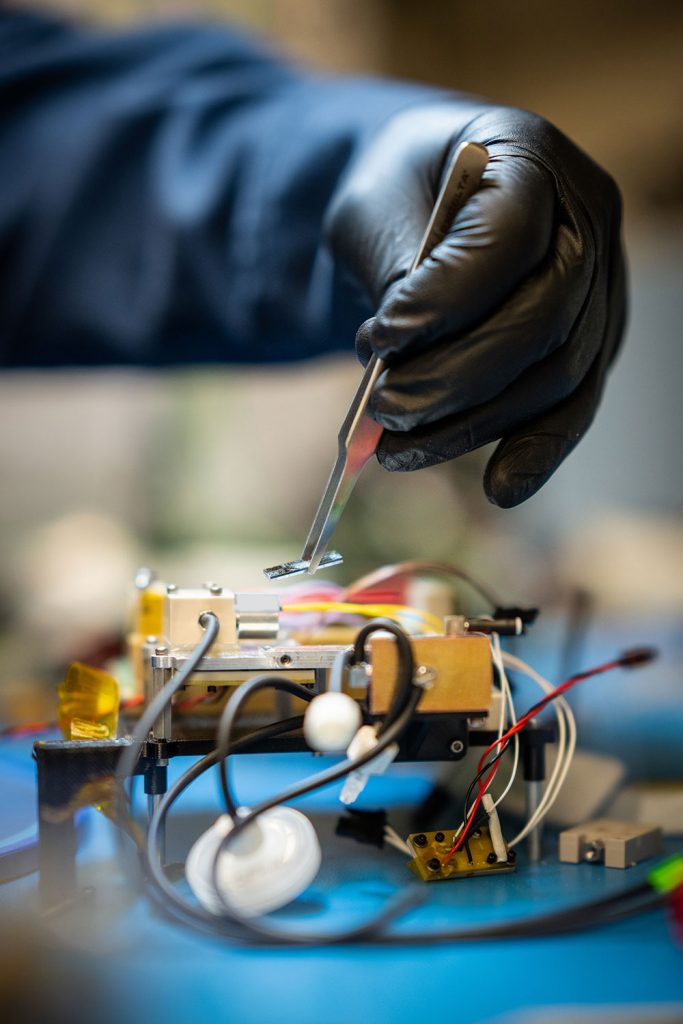
“We used a three-part system to do the analysis,” Philip said. “We split the analysis into multiple stages to do the collection, separation and identification of VOCs. Two of the components are made in Sandia’s Microsystems Engineering, Science and Applications silicon fabrication complex.”
The first Sandia-made microdevice serves as a “sponge” to soak up gases. The sponge or pre-concentrator, a silicon-based device slightly smaller than the inner loop of a mini-paper clip, collects VOCs from a bit of gauze that had been on a patient’s skin and holds onto them, letting the much smaller gases that make up air, such as oxygen, nitrogen and argon, flow through. After collecting gases from the gauze sample, the pre-concentrator was rapidly heated. The heat effectively “wrings” out the sponge, sending the VOCs into the next stage of the sensor. The pre-concentrator allows the device to detect even minuscule amounts of the gases of interest, Philip added.
The next stage, the separation stage, uses two miniaturized gas chromatography columns to separate the gases released from the pre-concentrator. Each of the columns is a tiny serpentine channel etched into a 1.2-by-1.2-inch square of silicon, Philip said. The two columns separate the gases based on two different chemical properties. Just like a doctor’s office separating out patients’ files by last name and then birthdate, using two different columns reduces the chances of a case of mistaken identity.
The third stage, the identification stage, uses a Sandia-made miniature ion-mobility spectrometer to detect the gases as they come out of the second column. This detector is sensitive enough to detect even tiny amounts of gases, such as the biological VOCs in this project or trace quantities of explosives, Philip said. For the prototype seizure detection system, it takes five minutes to analyze a sample from start to finish.
SEIZURE WARNING SYSTEM — Watch a video about the miniaturized sensor system and how it can mimic seizure-alert dogs in providing warnings of impending seizures. (Video by Ruth Frank)
Philip’s team also designed the microcontrol board that controls the various components in the silicon-based seizure gas detection sensor.
From the benchtop to the wrist
So far, Sandia and Know Biological have received four joint patents and have two other patent applications under review, Arnold and Philip said. Philip said the company has also licensed several Sandia technologies to test in this sensor.
The next step is to tweak the prototype sensor to sniff gases directly from someone’s skin, rather than from a bit of gauze that had been on their skin, Philip said. He doesn’t expect this to pose much challenge, but it is an important step before the system can be refined into a watch-like wearable sensor with the ability to collect samples throughout the day.
Then, the sensors can leave the lab and go home with people with epilepsy. Arnold expects to enroll patients in beta testing soon, with hopes of having the sensor on the general market by the end of 2024.
“To me, this test is the period at the end of the first full chapter on the microChemlab story,” Philip added. “Greg Frye-Mason envisioned this more than 25 years ago, and we’re now at a point where the system can be used as a medical device that could significantly improve the health and well-being of an individual. That’s really cool. The next chapter is getting it out of the lab and into the hands of healthcare providers and patients.”