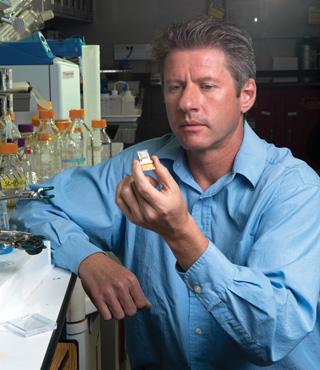
Ronen Polsky holds a prototype of a microneedle fluidic chip device able to selectively detect and painlessly measure electrolytes in the interstitial fluids that bathe skin cells. The device features nine sampling needles, each just 800 millionths of a meter (microns) in height, and beneath them, a fluidic channel that can draw interstitial fluid over nine gold disk electrodes. Each disk can be tailored to detect a different analyte. The visible rectangular gold pads are contacts. (Photo by Randy Montoya)
Soldiers on long missions, encased in tactical armor, could monitor their electrolytes with a diagnostic tool worn on the wrist and immediately detect and remedy deficiencies, thanks to a prototype device that Sandia researchers are patenting.
Electrolyte levels are key to optimizing health, strength, and awareness, not only for soldiers but for anyone who subjects the body to extremes. The ability to predict and upgrade the performance of long-distance runners or competitors in other strenuous sports would improve significantly if coaches could learn what’s happening physiologically while the athlete is exercising. The knowledge would help the self-aware athlete as well.
Electrolytes are crucial in carrying electrical impulses that tell the heart and other muscles when to contract or relax. Even non-athletes who feel poorly and try to navigate today’s complex medical system with its costly laboratory analyses might prefer a pain-free home diagnostic device that can analyze and continuously record electrolyte levels.
The Sandia researchers used various miniaturization techniques to shrink laboratory-scale equipment that analyzes various electrolyte levels on the spot down to a model that can fit in a palm or be worn on a wrist. The device, when commercially available, could decrease the time patients must spend in emergency rooms, lab testing facilities, or doctors’ offices.
Painless, noninvasive, long-term use
The device is painless because it employs micro-needles so tiny they can’t traumatize nerves when pressed into the skin, and samples only interstitial fluid (i.e. fluid between cells). Thus the device has the potential for long-term, noninvasive use.
“We’re proposing a minimally invasive way to move away from centralized laboratory testing,” says Ronen Polsky (1714), lead Sandia researcher on the project.
In a paper to be published as a cover feature in the June issue of Advanced Healthcare Materials (Wylie) and available online, Ronen, Sandia colleagues, and University of North Carolina/North Carolina State University graduate student Phil Miller describe using a fast-pulsed laser to create strong hollow microneedles that suck infinitesimal amounts of colorless fluid from just beneath the skin’s surface. The paper demonstrates that tiny amounts of potassium passed unhindered through the microneedle pores into a fluidic cartridge containing carbon electrodes. These measured the amount of this key electrolyte without being confused by the presence of other electrolytes in the fluid.
Miller says it’s easy to change the selectivity of the carbon electrodes to detect and measure other such electrolytes as sodium or calcium in the same device. “We want to make the device wearable, non-invasive, and with real-time readout to constantly measure things a doctor might normally order for laboratory tests,” he said.
University of New Mexico physician and researcher Justin Baca, who will lead human testing of the device, adds, “Development of this benchtop device into a handheld model for consumers and patients will be a true partnership between a clinician and an engineer.”
Sometimes sensor technologies work well, but problems arise when they are adapted to living systems, Baca said. “We’re trying to get at this problem from the beginning to develop the best needle geometry.”
Baca, with a background in physical chemistry and a practice in emergency medicine, says he has initial approval from UNM’s Human Research Protection Office review board to start tests. He’s interested, he says, because “it’s hard, using traditional methods, to take blood samples continuously.” Using only interstitial fluids is another matter entirely, he said.
The initial sensor work was funded by Sandia’s Laboratory Directed Research and Development program and the US Defense Threat Reduction Agency. Others working on the project include University of North Carolina/North Carolina State professor Roger Narayan.
“This is the future of personalized health care,” says Ronen. “These wearable technologies are just starting to come out in different forms. It’s inevitable that people will go there.”